In Psychology Today, they describe the “Anniversary Effect,” as a unique set of unsettling feelings, thoughts or memories that occur on the anniversary of a significant experience.
When the anniversary of my mom going into the hospital approached, I was hit with many emotions. I cried so many times that day grieving my life before and my relationship with my mom. My tears were over what she went thru and what we both lost over the last year.
My mom is an amazing mom and also my best friend. We spoke on the phone multiple times a day, sometimes for only a few minutes but often times at length. I could ponder life and she shared so much wisdom with me. She knew everything about me and she was the first to celebrate my accomplishments and never hesitated to call me on my shit.
“Trauma anniversaries can bring sadness as you grieve the life you had before trauma or what you’ve lost along the way” – Madeline Popelka
When she got home from the hospital I became her caregiver and no longer her daughter or friend. She came home with a feeding tube, a drain, and wasn’t able to walk out on her own. She could not be alone at any point. We hired caregivers to help and they were there every night and some days because I returned to work (remotely). She called them her babysitters. I called them my angels.

I lived with her for almost 6 weeks and only got to go home twice for a couple hours.
I can’t find words or paint a picture to explain that period in my life. It was the loneliest I have ever felt and I longed to talk to my best friend about everything going on. I was trying to work, manage her medicines, therapies, multiple doctor visits each week, and find her a place to live closer to me.

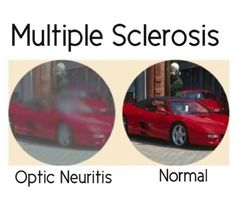
My mom is doing much better physically after additional procedures and set backs. She lived in assisted living for 4 months and now lives in independent living with her dog, Piper. Unfortunately due to the trauma and anesthesia she experienced, it left her with some cognitive damage. She suffers from short term memory loss and her ability to process concepts.
As I go thru the anniversary of the trauma of last year, I also hold gratitude in my heart. I am grateful she survived last year and so grateful for the support of my friends and family. My mom and our relationship may never be the same again, but we are finding our new normal. That includes more laughter, less tears, a lot of eating out, and showing her how to use electronics.